DNP 801 Topic 7 DQ1
Topic 7: Chronic Disease
Objectives:
1. Assess the impact of chronic disease and client demand on expenditures and resources.
2. Propose methods to use evidence-based data sources on innovative approaches to care of patients with chronic disease.
Topic 7 DQ 1
What is the impact of chronic disease on both increased health care expenditures and wasted
resources? Do genetics play a role? How can the doctoral-prepared nurse apply this information in practice? Explain. Support your rationale with a minimum of two scholarly sources.
Topic 7 DQ 2
Identify a method that uses evidence-based data to support new or innovative ways to care for patients with chronic disease. What are the anticipated outcomes of employing this method and methods like it? How can the doctoral-prepared nurse apply this information in practice? Explain. Support your rationale with a minimum of two scholarly sources.
Sample 1 Topic 7 DQ1
According to CDC, chronic illnesses such as heart disease, cancer, diabetes, stroke, and chronic lung disease account for 70% of deaths and 75% of health care costs. Although efforts in managing chronic illness typically originate in the health care system, governmental and community-based public health organizations play an important role in helping people with chronic illness maintain optimal health. The consequences of chronic illness include physical, mental, and social consequences that affect patients and their family members, friends, and caregivers. A person with arthritis may have all 3 consequences: physical, such as chronic pain; mental, such as depression; and social, such as an inability to work. Complicating our ability to track, treat, and manage chronic illness is the fact that commonly used outcome measures are not concordant for a given illness. Some illnesses, such as diabetes, have a great effect on care use, while others, such as arthritis, have their greatest effect on mobility, employment, and economic outcomes.
Genetic predisposition plays a crucial role in the development of chronic disease. The presence of genetic predisposition and environmental factors enhance the chances of developing the disease. The doctoral prepared nurse can help patient understand the benefits of bundled care services in order to reduce healthcare expenditure on both long term and acute symptoms. The knowledge on the genetic predisposition to disease is also helpful in genetic counselling in order to improve the chances of future generations in developing the disease.
Reference
Maresova, P., Javanmardi, E., Barakovic, S. et al. Consequences of chronic diseases and other
limitations associated with old age – a scoping review. BMC Public Health 19, 1431 (2019). https://doi.org/10.1186/s12889-019-7762-5
Sample 2 Topic 7 DQ1
Increasing population in aging and increased life expectancy are causing high health expenditures and increase importance of the healthcare system. Efficient spending on healthcare is required to reduce unnecessary utilizations and focused on treatment and management of acute disease. According to World Health Organization (WHO), premature mortality from non-communicable diseases, also known as chronic diseases, accounted for 52% of global deaths under the age of 70 years in 2012. Chronic disease is usually defined as a disease that lasts for more than a year
and requires ongoing or continuous management. WHO reported that chronic diseases are classified into four major categories: cardiovascular disease, cancer, chronic respiratory disease, and diabetes. Chronic diseases are caused by a number of complex factors, such as genetic, physiological, environmental, and behavioral factors. Continuity of care for chronic diseases, which indicates regularity of visiting a primary care doctor, may increase healthcare expenditure in the short-term by increasing direct medical costs with spending more on prescription drugs. Chronic diseases increases, patients should have a regular site to improve their health status through steady follow-up for reducing total healthcare expenditures and to decrease inefficient healthcare utilizations.
There are many possible causes of human disease, family history is often one of the strongest risk factors for common disease complexes such as cancer, cardiovascular disease, diabetes, autoimmune disorders, and psychiatric illnesses. A person inherits a complete set of genes from each parent, as well as a vast array of cultural and socioeconomic experiences from his/her family. Technological advances in high-throughput genotyping have allowed the direct examination of specific genetic differences among sizable numbers of people. Genetic association techniques are often the most efficient approach for assessing how specific genetic variation can affect disease risk.
Genetic variation impacts all cellular, biochemical, physiological, and morphological aspects of a human being and genes whose variability controls how much or how little a person is likely to be responsive to the environmental risk factors that are associated with disease risk.
Nurses, the most trusted health professionals and, make unique contributions to the field of human genetics and genomics and complement the work of other health care providers to improve the health of the public. Health care benefits greatly from the unprecedented and ongoing work elucidating the genetic/genomic basis of health, illness, disease risk, and treatment response. nursing profession is a pivotal provider of quality health care services and is essential to closing the gap between research discoveries that are efficacious to health care and their successful
adoption to optimize health.
References
Centers for Disease Control and Prevention. Chronic Disease Prevention and Health Promotion, Chronic Disease Overview, 2017. URL: https://www.cdc.gov/chronicdisesase/overview/.
Global Status Report on Noncommunicable Diseases 2014: Attaining the Nine Global Noncommunicable Diseases Targets: A Shared Responsibility. [(accessed on 21 August 2018)]; Available online: http://www.who.int/nmh/publications/ncd-status-report-2014/en
Pinkovskiy ML. The impact of the manage care backlash on health care costs: evidence from state regulation of managed care cost containment practices. New York: Federal Reserve Bank of New York; 2019.
Sample 1 Topic 7 DQ2
EBP, otherwise recognized as evidence-based practice, is the judicious and conscientious utilization of specialized clinical expertise alongside current best evidence and patient values to guide health care decisions. To implement evidence-based practice, practitioners must first identify practices and programs tested and shown effective (Abidi, 2017). Moreover, leaders of nursing backgrounds enact successful EBP integration through attaining generalized leadership awareness and recognizing the importance of being knowledgeable about a proposed change, partnering with a team of staff ready for the change, engaging the help of mentors or change agents at the unit level. EBP proves its indispensable nature through how it aims to provide efficacy within patient outcome improvement (Abidi, 2017). Patients expect the most effective care based on the best available evidence. It is believed that with improved healthcare delivery that focuses on evidence-based management therapies, cases of hospital readmissions can be reduced significantly (Abidi, 2017).
Hypothesis: “Healthcare professionals can implement existing evidence-based management therapies and develop strategies to prevent hospital readmission for patients diagnosed with
congestive heart failure (CHF).”
According to Davidson et al. (2015), it is essential to possess standardized practice concerning congestive heart failure management. The current approach enabling doctors to embrace differing methods rooted in biased decisions does not assume a responsible stance within a modern society where advanced technology has enhanced health delivery. MAP, known as multidisciplinary action plans, are some evidence-based therapies that are increasingly becoming popular in managing congestive heart failure (Davidson et al., 2015). Designed to provide the framework for inpatient management of CHF, MAP is a structured nursing plan for inpatients. It is recommended that before a CHF patient is discharged from the hospital. A cardiologist, nephrologist, dietician, family practitioner/PCP, and a hospital representative should be present and give their approval and home health referral for medication management (Davidson et al., 2015). The primary objective is to ensure that when the patient leaves the hospital, the entire medical team will be confident that all the necessary factors are considered to minimize the chances of hospital readmissions (Davidson et al., 2015).
Doctorally prepared nurses to promote the uptake of evidence by developing the knowledge and skills of clinical nurses through role modeling, teaching, clinical problem-solving, and facilitating change (Anderson, 2015). They must be prepared to assume the responsibility and accountability to make complex health care decisions based on findings from rigorous or high-quality research reports, clinical expertise, and patient perspectives. The implementation of EBP enables DNP-prepared nurses to apply data-backed solutions that incorporate clinical expertise and current research into the decision-making process (Anderson, 2015). As a result, to produce positive patient outcomes by integrating the best research evidence, clinical expertise, and patient preferences (Anderson, 2015).
References
Abidi, S. (2017). A knowledge-modeling approach to integrate multiple clinical practice guidelines to provide evidence-based clinical decision support for managing comorbid
conditions. Journal of Medical Systems, 41(12), 1-19.
Anderson, B. A. (2015). Caring for Vulnerable Populations: The Role of the DNP-Prepared Nurse. Caring for the Vulnerable: Perspectives in Nursing Theory, Practice and Research, 441.
Davidson, P. M., Newton, P. J., Tankumpuan, T., Paull, G., & Dennison-Himmelfarb, C. (2015).
Multidisciplinary management of chronic heart failure: principles and future trends. Clinical therapeutics, 37(10), 2225-2233.
Sample 2 Topic 7 DQ2
expected for routine visits. The elder population in Alaska is one of the most vulnerable populations. They live far from medical facilities and may not have providers in the village. Living with chronic illness and so far from care makes it difficult to maintain proper health. Over the last two years, we have seen a significant uptake in the use of telemedicine. This has given the elder population and those who have little access to healthcare a valuable and necessary option. Studies have concluded that patients and providers have positive reviews on the use and found it very effective. This is most significantly seen in those with chronic illness where transport is difficult (Jordan et al., 2021)
The Alaska Federal Care Access Network (AFHCAN) telehealth systems have deployed over 253 locations throughout Alaska. Patients are able to go to the village clinic or health aid office and receive a complete medical exam. The system uses video-assisted devices to listen to lung sounds, look at ears or eyes, check vital signs, and much more. The increased ability to use telehealth as an actual provider visit has brought health care to patients that would have otherwise had to take a
commercial flight to see a doctor. (Hudson, n.d.)
The DNP-prepared nurse is able to use this information to educate their patients on its use before
leaving inpatient or clinic visits. The nurse can help the patients understand what to expect, how to use it, where to go, and when to seek care. Having no one with a solid medical background hooking you up to a machine that looks alien can be intimidating and cause individuals to put off seeking care. With chronic illness, it is imperative to have routine visits.
References
Hudson, H. (n.d.). Rural Telemedicine and Telehealth: The Alaskan Experience.
Institute of Socal and Economic Research. http://www.akleg.gov/basis/get_documents.asp?session=29&docid=52439
Jordan, D., Jessen, C. M., & Ferucci, E. D. (2021). Views of patients and providers on the use of
telemedicine for chronic disease specialty care in the alaska native population. Telemedicine and e-Health, 27(1), 82–89. https://doi.org/10.1089/tmj.2019.0284
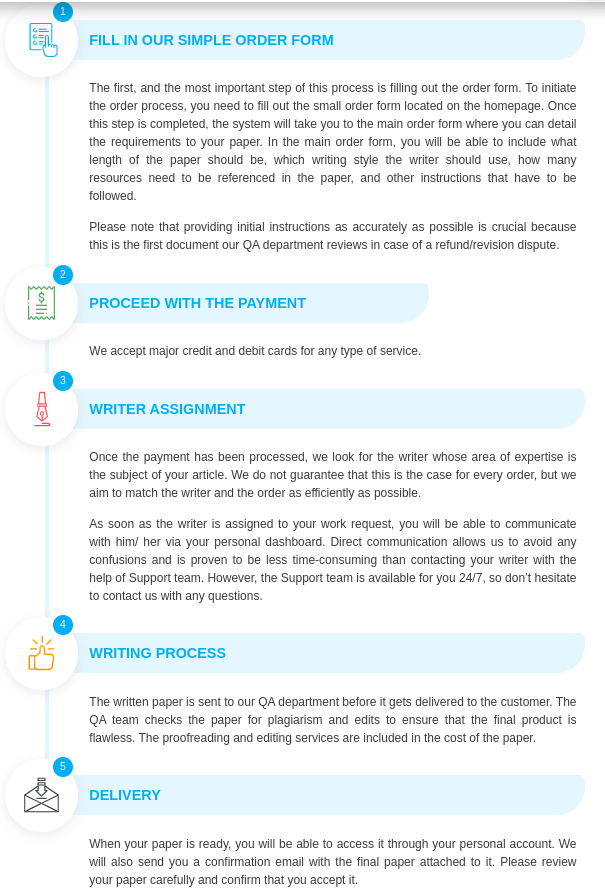
Our team of expert nursing writers at Nursing Assignment Service can help you with your DNP 801 Topic 7 DQ1, place your order here.